CareJourney Overview
CareJourney drives network growth and care coordination through its healthcare analytics solutions. Providers and payers can leverage comprehensive data to enhance clinical performance and make informed contracting decisions. The platform supports Accountable Care Organizations (ACOs) in achieving significant savings, reportedly 1.5 times more than typical outcomes. It helps identify patient leakage, strengthen referrals, and improve provider performance. By offering insights into market and cohort intelligence, CareJourney aids in better managing at-risk populations. The solutions are grounded in an extensive longitudinal data set, positioning healthcare professionals to expand their value-based care knowledge and improve patient outcomes.
Use Cases
Customers recommend Lead Analytics, Competitive Intelligence, Collaboration, as the business use cases that they have been most satisfied with while using CareJourney.
Business Priorities
Improve Efficiency and Enter New Markets Internationally Or Locally are the most popular business priorities that customers and associates have achieved using CareJourney.
CareJourney Use-Cases and Business Priorities: Customer Satisfaction Data
CareJourney, Adobe Marketo Measure (formerly Bizible), Adjust, Calibermind, Attribution, etc., all belong to a category of solutions that help Marketing Attribution. Each of them excels in different abilities. Therefore, determining the best platform for your business will depend on your specific needs and requirements.
CareJourney offers healthcare analytics solutions to aid providers and payers in making informed decisions. Network growth and care coordination are key focus areas.
CareJourney Customer wins, Customer success stories, Case studies
How efficiently Does CareJourney manage your Lead Analytics?
Why is CareJourney the best choice for Competitive Intelligence?
What benefits does CareJourney offer for Collaboration?
How does CareJourney facilitate Contract Management?
11 buyers and buying teams have used Cuspera to assess how well CareJourney solved their Marketing Attribution needs. Cuspera uses 240 insights from these buyers along with peer reviews, customer case studies, testimonials, expert blogs and vendor provided installation data to help you assess the fit for your specific Marketing Attribution needs.
CareJourney Competitors
CareJourney Features
- Low
- Medium
- High
| FEATURE | RATINGS AND REVIEWS |
|---|---|
| Custom Reports | Read Reviews (61) |
| Analytics | Read Reviews (69) |
| CAPABILITIES | RATINGS AND REVIEWS |
|---|---|
| Custom Reports | Read Reviews (61) |
| Analytics | Read Reviews (69) |
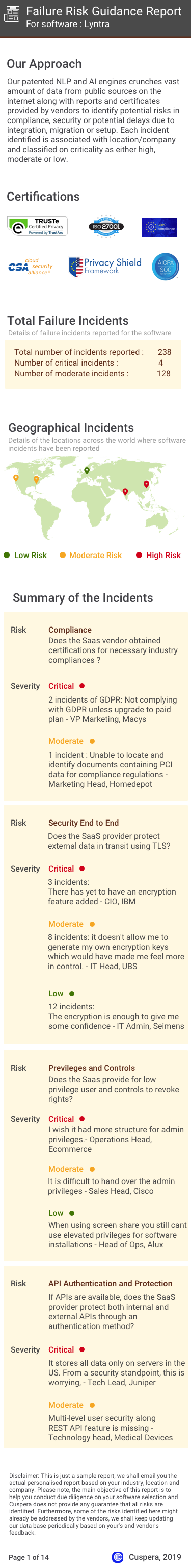
Software Failure Risk Guidance
?for CareJourney
Overall Risk Meter
Top Failure Risks for CareJourney
CareJourney Profile
Company Name
CareJourney
Company Website
https://carejourney.com/HQ Location
3865 Wilson Blvd, Suite 225, Arlington, VA 22203, US
Employees
51-100
Social
Financials
SERIES A